CLINICAL TECHNIQUE | https://doi.org/10.5005/jp-journals-10024-2614 |
A Consolidated Pulp Test System Including Flowmetry, Pulse Oximetry, and Thermometry
1Department of Endodontics, Faculty of Dentistry, Mashhad University of Medical Sciences, Mashhad, Islamic Republic of Iran
2Department of Biomedical Engineering, Faculty of Power and Computer, University of Tarbiat Moadares, Tehran, Islamic Republic of Iran
3Department of Medical Equipments, Imam Reza Hospital, Mashhad University of Medical Sciences, Mashhad, Islamic Republic of Iran
4–6Department of Conservative Dentistry, Showa University Dental Hospital, Tokyo, Japan
7Faculty of Dentistry, University of Toronto, Toronto, Canada; Department of Dentistry, Mount Sinai Hospital, Toronto, Canada
Corresponding Author: Hamid Jafarzadeh, Department of Endodontics, Faculty of Dentistry, Mashhad University of Medical Sciences, Mashhad, Islamic Republic of Iran, Phone: +98-51-38829501, e-mail: JafarzadehBH@mums.ac.ir
How to cite this article Jafarzadeh H, Iusefipour F, et al. A Consolidated Pulp Test System Including Flowmetry, Pulse Oximetry, and Thermometry. J Contemp Dent Pract 2019;20(7):873–877.
Source of support: National Elite Foundation of Iran
Conflict of interest: None
ABSTRACT
Aim: The aim of this study is to report manufacturing a consolidated pulp test system that includes thermometry, flowmetry, and pulse oximetry.
Background: The ideal method for the evaluation of pulp vitality should be objective, noninvasive, easy to use, reliable, and painless. Currently, the most commonly used tests (such as electricity, heat, and cold tests) depend on patients’ sensibility and are highly subjective. They only measure a neural response and do not indicate the actual biologic status of the pulp. It has, therefore, been suggested that vitality tests such as flowmetry, pulse oximetry, thermometry, and photoplethysmography be used. Some research has been done on these systems; however, their high costs and space need to maintain all of them that have been obstacles to their use.
Technique: This report describes designing and manufacturing a novel system for evaluating pulp vitality involving the use of three methods (flowmetry, pulse oximetry, and thermometry) combined in a single small system using only two probes.
Conclusion: The consolidated pulp tests system may be accurate in determining the pulp vitality. However, after clinical use, some changes may be necessary for improvement of the system.
Keywords: Endodontics, Flowmetry, Pulp test, Pulp vitality, Pulse oximetry, Thermometry.
INTRODUCTION
An essential part of the evaluation of pulp status is the use of pulp sensibility tests. These tests include thermal tests (cold and hot) and the electric pulp test. The advantages of these tests are their simplicity and low cost and; hence, they are commonly used tests in endodontic practice. However, sensibility tests are limited as they only assess if pulpal nerve fibers can respond to electrical/heat/cold stimulus when applied to the outer surface of the tooth. These tests do not provide information about the pulp’s vascular supply,1,2 in particular, in case of open-apex or traumatized teeth, and teeth that have been involved in orthognathic surgery. For example, for recently traumatized teeth, temporary paresthesia of nerves may reduce the effectiveness and reliability of the sensibility tests. Therefore, such teeth, even though they have intact vasculature, have compromised neural responses and, hence, may not respond (or provide a valid response) to sensibility tests.1 This is currently posing a dilemma in diagnosis and timely initiation of the treatment, if indicated.3 Hence, it can be argued that the available pulp sensibility tests cannot be considered as a true vitality test, the one that actually assesses the blood vessels or blood flow.
There have been some previous attempts in proposing pulp vitality tests including pulse oximetry,3 laser Doppler flowmetry,4 tooth temperature measurement,5 and photoplethysmography.6 Pulse oximetry is commonly used for medical purposes. It is a noninvasive technique for measuring oxygen saturation in different tissues such as the pulp.3,7,8 In this method, a probe containing two light-emitting diodes for transmitting red light (to measure the absorption of oxygenated hemoglobin) and infrared light (to measure the absorption of deoxygenated hemoglobin) is used. Different amounts of red and infrared lights are absorbed by oxygenated and deoxygenated hemoglobin. The light is received by a special photodetector diode connected to a microprocessor. The relationship between the pulsatile changes in absorption of red and infrared lights is measured by the microprocessor to show the oxygen saturation.3,9 A major shortcoming of this technique in endodontic diagnosis is that no prefabricated dental probe is accessible in the market.9
Flowmetry has been shown as a reliable technique for the measurement of pulpal blood flow through measuring the blood volume or the velocity of red blood cells.10–15 However, difficulty in its use in clinical practice and its high cost has delayed it from being a routine test for pulp vitality evaluation.4
The measurement of tooth temperature (through using thermistors, a thermocouple, cholesteric liquid crystals, miniature thermometers, and infrared thermography5) has been shown to be another suitable method that may indicate the status of pulp vasculature.16–21 However, these tests have not been routinely used because they are time consuming, costly, or bulky in nature (see earlier comment). We propose a simplified system, combining these three systems, at a smaller size and lower cost, would be a helpful chairside diagnostic aid in endodontics. Hence, the aim of this project is to design and manufacture a system that is capable of performing all three tests using one small-size system while using only two probes—a feature that would reduce the time for testing, cost, and bulk of the systems.
MATERIALS AND METHODS
Our assembled diagnostic tool consisted of three systems including infrared flowmeter, pulse oximeter, and thermometer. The specific parts are described as below.
Pulse Oximeter
A finger pulse oximeter module is small and simple to use in combination with a microprocessor. We used a prepared module, consisting of two emitting diodes: one transmitter sensor and one photodetector diode receiver sensor. These sensors work when the humidity of the surface is lower than 85%. This can be achieved by drying the surface of the tested teeth by using air blasting. The frontal and lateral view of the pulse oximeter sensor is shown in Figue 1 and its circuit is shown in Figure 2.
Flowmeter
To measure the pulpal blood flow, the infrared transmitter–transceiver circuit was used. This kind of circuit has been previously used in sphygmography.22,23 The operation of this sensor is based on the changes in the light volume. The sensor detects the passing of light through the pulp and produces a waveform. Using this circuit, and in the first step, the changes of the volume of the passing blood in the pulp can be measured. The sensors used for this purpose were infrared sensors that work on the basis of the light intensity. The sensor transmits the infrared light by an explicit intensity and, then, according to the changes in the volume of the passing blood, the receiver shows different intensities. Using this circuit, transmitted light and its difference in different statuses such as systole and diastole can be measured. The light sensor used in the system was CNY70; this is a reflective sensor that includes an infrared emitter and phototransistor in a package which blocks visible light. It can measure the volume of the passing blood in each heartbeat. So with the changes in blood volume—which decrease or increase in each systolic or diastolic pulse—the intensity of the received light differs and so a pulse proportional to the heartbeat on the oscilloscope can be seen. For measurement of the blood flow, the integral of the transmitted pulse related to its reference line is measured and then divided by the period of pulse. In this way, the blood flow is measured. The output of the transmitter–receiver (as an analog waveform) circuit is sent to the microcontroller and digitized and the calculations then done. The final result, which is the pulpal blood flow, is then displayed on the liquid crystal display (LCD) (Fig. 3).

Fig. 1: Frontal and lateral view of the pulse oximeter sensor

Fig. 2: Circuit of the pulse oximeter
Thermometer
LM35 thermal precision IC temperature sensors (with dimensions of <1 cm, and a supply voltage of 5 V) were used for thermometry (Fig. 4). The result of the sensor displays on the LCD. The output voltage is linearly proportional to the centigrade temperature. It does not require any external calibration to provide accuracies of ±1/4°C at the room temperature and ±3/4°C over a full −55 to +150°C temperature range. Low cost is a major advantage of these sensors. It draws 60 μA from its supply, so it surprisingly has very low self-heating lower than 0.1°C in still air. In this plan, the desired temperature interval is 35–45. The module of thermometer is <6 cm long, making the device portable.

Fig. 3: View of the final circuit and LCD

Fig. 4: The dimensions of the thermometer sensor
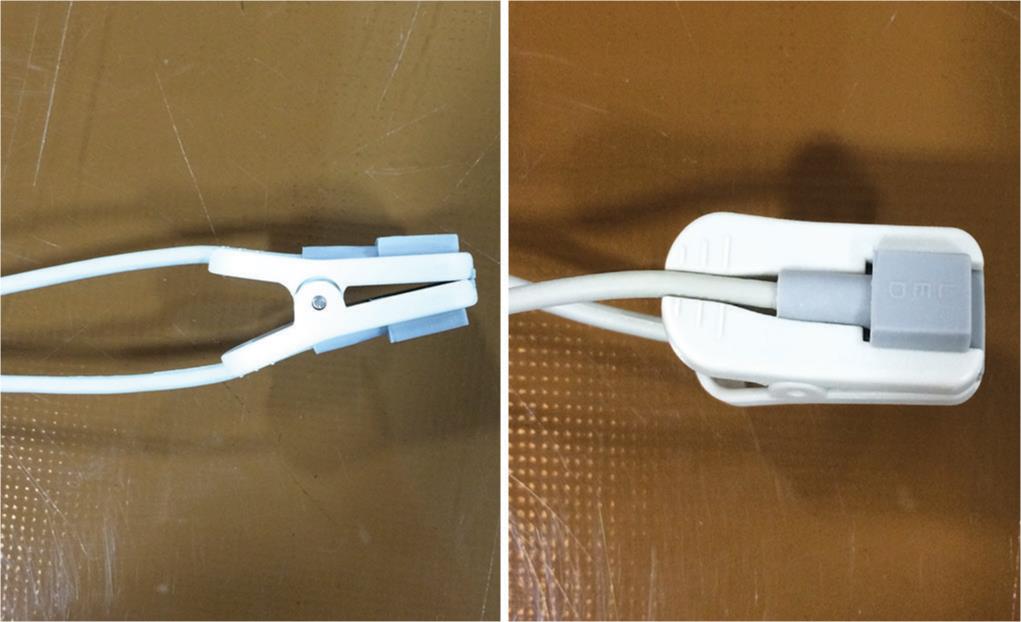
Fig. 5: Fabricated probes for pulse oximetry testing
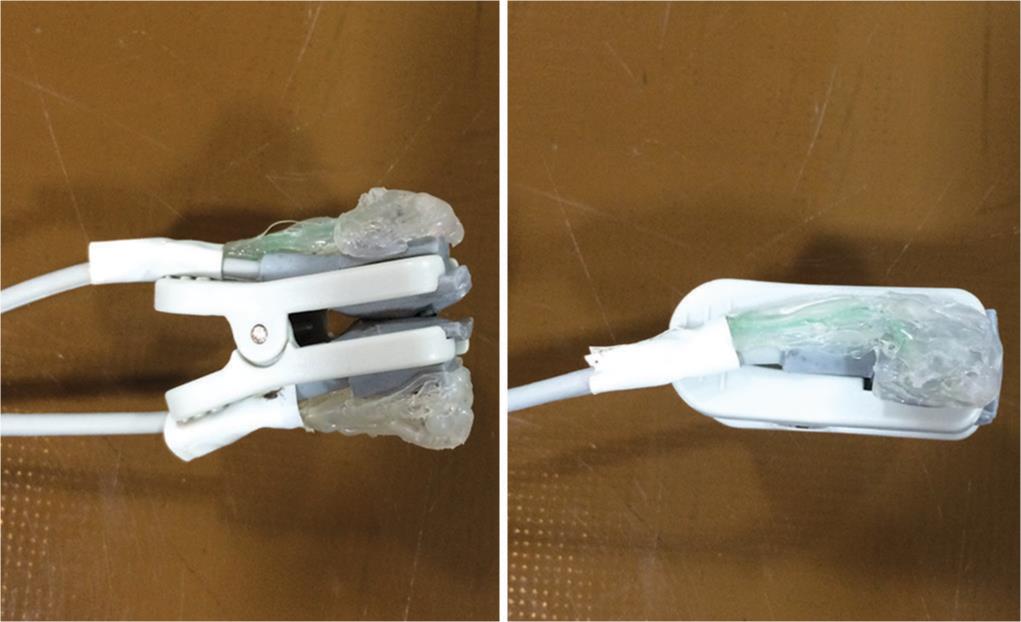
Fig. 6: Fabricated probes for flowmetry and thermometry testing
Microprocessor
A 32-bit micro-controller with the ARM core (ARM7 series/Cortex-M3—LPC1768)24 is the central core of the system. This small yet user-friendly compilers processor has various embedded accessories (e.g., 64 KB SRAM, 512KB Flash, enough pin for LCD or its driver connecting, USB 2.0 full-speed compatible connector). It uses high-level coding languages (C++ Keil)25 to promptly process data obtained from the thermometer and the flowmeter.
LCD
For our proposed device, an HD44780 Character LCD, with a 16 × 2 display (2 lines and 16 characters per line), has been used. This LCD has 16 pins, but only 11 of them are for communication. These pins are for connecting to the microcontroller. Output LCD display is “Flow” and “Temp.” The pulse oximeter has a separated LCD in package with a module.
Probes
Because of the size of the sensors compared with normal teeth size, we used one probe for the pulse oximetry and a second one for joint flowmetry and thermometry. This means that the results of the flowmetry and thermometry were obtained simultaneously whereas for obtaining the result of the pulse oximetry, the first probe has to be removed from the tooth surface and the probe of the pulse oximetry replaced on the outer surface of the tooth; however, because of bifurcating the probe from the last segment (10 cm to end), the sensors are too close. This decreases the time needed to replace sensors. For obtaining the best adaptation to the anatomy of the anterior and premolar teeth, the custom-made probes were prepared to be similar to finger probes of the pulse oximeters (Figs 5 and 6). The maximum and minimum dimensions of these teeth were obtained from Wheeler’s Dental Anatomy, Physiology, and Occlusion Atlas.26
Assembled System
We used Altium PCB Design Software (Altium, CA, USA), to design two PCB boards: thermometer/flowmeter board and pulse oximeter board. To reduce the dimensions of the device, LCDs were mounted in free space on the board. Finally, a box for the device with a 1.5-m cable probe was built. The power supply was 5 V DC; however, a mini-transformator was built so that 110–220 V AC can be easily used. The final assembled size of 15 × 15 cm and a low weight of 250 g make this diagnostic aid very portable.
DISCUSSION
Only a test that actually measures or assesses pulp blood flow can be called a vitality test.4 As technology has increased, some aspects of dental practice and its related devices and equipment need to be revised to obtain more precise diagnoses and treatments. The main purpose of this project was to manufacture a unique pulp test that merges three vitality tests (namely pulse oximeter, thermometer, and flowmeter) to provide an accurate diagnosis, while at the same time, it is small, not costly and reduce the time needed for vitality testing.
Testing vascular supply relies on the passage of light through a tooth. Flowmetry is reproducible and has been considered as the gold standard in determining the pulpal blood flow but only under carefully controlled conditions.27 The value of this system has been well documented, but its high cost and difficulty of use in clinical practice have delayed its routine usage. Moreover, factors such as probe design, holder characteristics, flowmeter characteristics, gingival isolation devices, the position of the probe, heartbeat-synchronous oscillations, and age-related changes, may significantly influence its results.4
Diagnosing teeth with vital pulp by temperature measurement may also provide valuable information on the integrity of the underlying pulp. Some authors have found no differences between the temperatures of teeth with nonvital and vital pulp.28–34 However, others35–37 found that teeth with nonvital pulp have lower temperatures than teeth with vital pulp. Many factors may influence the results of the temperature measurement procedure which means that it should be performed in completely controlled conditions-care must be taken to control as many variables as possible when studying temperature.5
The critical requirement for using the pulse oximeter in dentistry is that the sensors should conform to the shape, size, and anatomy of the tooth, and that the LED and the photodetector should be parallel to each other, so that all the light emitted by the LED sensor is received by the photodetector sensor. If the sensor cannot adapt to the shape and size of the crown, reliable results may not be obtained. There are no pulse oximeter probes specific for teeth in the market. This constitutes a limitation of the general use of the pulse oximeter in dentistry. The probes used for a finger or an infant’s foot readings cannot accommodate the tooth structure, because of the beam distortion, so some researchers have successfully used modified finger probes or adapted the instrument to the teeth to demonstrate the system reliability in the diagnosis of pulp vitality.3 Some other innovative probes have been used by other researchers such as Noblett et al.,8 Kahan et al.,38 Goho,39 and Gopikrishna et al.40,41 As stated; however, special probes are not accessible in the dental market and this is a major limitation in introducing these systems into diagnostic procedures in endodontics. Through this project we were able to make specific dental probes for application in pulse oximetry, thermometry, and flowmetry.
Our inexpensive compact and accurate diagnostic aid has the potential for widespread use in endodontic diagnosis. Our next step is to conduct a clinical study to evaluate its diagnostic accuracy in assessing pulp vitality.
CONCLUSION
The consolidated pulp tests system may be accurate in determining the pulp vitality. However, after clinical use, some changes may be necessary for improvement of the system.
CLINICAL SIGNIFICANCE
This system may help clinicians and researchers to obtain more reliable results—as well, there may be other advantages such as decreasing the costs and the space needs required to maintain all three systems, separately.
ACKNOWLEDGEMENTS
This project has been supported by the National Elite Foundation of Iran. The authors would like to thank the Vice Chancellor of Mashhad University of Medical Sciences for his technical support (Protocol number: 88765). They also want to acknowledge Prof Paul A Rosenberg for his beneficial comments on this work.
REFERENCES
1. Jafarzadeh H, Abbott PV. Review of pulp sensibility tests. Part I: general information and thermal tests. Int Endod J 2010;43:738–762. DOI: 10.1111/j.1365-2591.2010.01754.x.
2. Jafarzadeh H, Abbott PV. Review of pulp sensibility tests. Part II: electric pulp tests and test cavities. Int Endod J 2010;43:945–958. DOI: 10.1111/j.1365-2591.2010.01760.x.
3. Jafarzadeh H, Rosenberg PA. Pulse oximetry: review of a potential aid in endodontic diagnosis. J Endod 2009;35:329–333. DOI: 10.1016/j.joen.2008.12.006.
4. Jafarzadeh H. Laser Doppler flowmetry in endodontics: a review. Int Endod J 2009;42:476–490. DOI: 10.1111/j.1365-2591.2009.01548.x.
5. Jafarzadeh H, Udoye CI, et al. The application of tooth temperature measurement in endodontic diagnosis: a review. J Endod 2008;34:1435–1440. DOI: 10.1016/j.joen.2008.09.011.
6. Miwa Z, Ikawa M, et al. Pulpal blood flow in vital and nonvital young permanent teeth measured by transmitted-light photoplethysmography: a pilot study. Pediatr Dent 2002;24:594–598.
7. McMorrow RC, Mythen MG. Pulse oximetry. Curr Opin Crit Care 2006;12:269–271. DOI: 10.1097/01.ccx.0000224873.16700.78.
8. Noblett WC, Wilcox LR, et al. Detection of pulpal circulation in vitro by pulse oximetry. J Endod 1996;22:1–5. DOI: 10.1016/S0099-2399(96)80226-3.
9. Dastmalchi N, Jafarzadeh H, et al. Comparison of the Efficacy of a Custom-made Pulse Oximeter Probe with Digital Electric Pulp Tester, Cold Spray, and Rubber Cup for Assessing Pulp Vitality. J Endod 2012;38:1182–1186. DOI: 10.1016/j.joen.2012.06.012.
10. Yeh Y, Cummins HZ. Localized fluid flow measurements with an He-Ne laser spectrometer. Appl Phys Lett 1964;4:176–178. DOI: 10.1063/1.1753925.
11. Gazelius B, Olgart L, et al. Non-invasive recording of blood flow in human dental pulp. Endod Dent Traumatol 1986;2:219–221. DOI: 10.1111/j.1600-9657.1986.tb00148.x.
12. Gazelius B, Olgart L, et al. Restored vitality in luxated teeth assessed by laser Doppler flowmeter. Endod Dent Traumatol 1988;4:265–268. DOI: 10.1111/j.1600-9657.1988.tb00645.x.
13. Olgart LM, Edwall B, et al. Neurogenic mediators in control of pulpal blood flow. J Endod 1989;15:409–412. DOI: 10.1016/S0099-2399(89)80173-6.
14. Ebihara A, Tokita Y, et al. Pulpal blood flow assessed by laser Doppler flowmetry in a tooth with a horizontal root fracture. Oral Surg Oral Med Oral Pathol Oral Radiol Endod 1996;81:229–233. DOI: 10.1016/S1079-2104(96)80420-3.
15. Yanpiset K, Vongsavan N, et al. Efficacy of laser Doppler flowmetry for the diagnosis of revascularization of reimplanted immature dog teeth. Dent Traumatol 2001;17:63–70. DOI: 10.1034/j.1600-9657.2001.017002063.x.
16. Howell RM, Duell RC, et al. The determination of pulp vitality by thermographic means using cholesteric liquid crystals. A preliminary study. Oral Surg Oral Med Oral Pathol 1970;29:763–768. DOI: 10.1016/0030-4220(70)90275-6.
17. Stoops LC, Scott D.Jr Measurement of tooth temperature as a means of determining pulp vitality. J Endod 1976;2:141–145. DOI: 10.1016/S0099-2399(76)80011-8.
18. Banes JD, Hammond HL. Surface temperatures of vital and nonvital teeth in humans. J Endod 1978;4:106–109. DOI: 10.1016/S0099-2399(78)80199-X.
19. Fanibunda KB. A laboratory study to investigate the differentiation of pulp vitality in human teeth by temperature measurement. J Dent 1985;13:295–303. DOI: 10.1016/0300-5712(85)90024-7.
20. Fanibunda KB. The feasibility of temperature measurement as a diagnostic procedure in human teeth. J Dent 1986;14:126–129. DOI: 10.1016/0300-5712(86)90077-1.
21. Fanibunda KB. Diagnosis of tooth vitality by crown surface temperature measurement: a clinical evaluation. J Dent 1986;14:160–164. DOI: 10.1016/0300-5712(86)90018-7.
22. Nafisi V, Sakhavi S. Designing equipment for monitoring and analyzing the pulse signal based on the Iranian traditional medicine. 4th Iranian Conference on eHealth and ICT Application in Medical Sciences, Mashhad, 2011.
23. Nafisi V. Designing and manufacturing pulse-meter for using in traditional medicine. Iranian Research Organization for Science and Technology 2013.
24. LPC1768 user manual, available online from: http://www.nxp.com/documents/user_manual/UM10360.pdf.
25. Yousefipoor F, Mirhadi M, et al. Device Design and Manufacturing for Measurement of Kinematic Specification of Hand Movement. Majlesi Journal of Multimedia Processing 2013;4(2):1–6.
26. Ash M, Nelson SJ. Wheeler’s Dental Anatomy. Physiology, and Occlusion,St. Louis: Saunders, 2010.
27. Evans D, Reid J, et al. A comparison of laser Doppler flowmetry with other methods of assessing the vitality of traumatised anterior teeth. Endod Dent Traumatol 1999;15:284–290. DOI: 10.1111/j.1600-9657.1999.tb00789.x.
28. Crandell CE, Hill RP. Thermography in dentistry: a pilot study. Oral Surg Oral Med Oral Pathol 1966;21:316–320. DOI: 10.1016/0030-4220(66)90064-8.
29. Brown AC, Goldberg MP. Surface temperature and temperature gradients of human teeth in situ. Arch Oral Biol 1966;11:973–982. DOI: 10.1016/0003-9969(66)90199-3.
30. Hartley JL, Stanfill DF, et al. Thermography of the human dentition. SAM-TR-67-57, USAF School of Aerospace Medicine 1967; 1–40.
31. Stanfill DF, Plakun BD. Feasibility study, thermography of human dentition. Barnes Engineering Co., Project 3812. Air Force Project Task no. 799601. 1966.
32. Herrmann M. Temperaturverhaltnisse an der Mundschleimhaut der Zunge und er Zahnen. Dtsch Zahnaerztl Z 1953;8:539–543.
33. Goldberg M, Brown AC. Human tooth surface temperature. Physiologist 1965;8:175.
34. Baumann G. Temperaturmessungen an vitalen und devitalen Zahnen. Inaugural dissertation.Mainz: Johannes Gutenberg Universitat, 1952.
35. Stoops LC, Scott D.Jr Measurement of tooth temperature as a means of determining pulp vitality. J Endod 1976;2:141–145. DOI: 10.1016/S0099-2399(76)80011-8.
36. Banes JD, Hammond HL. Surface temperatures of vital and nonvital teeth in humans. J Endod 1978;4:106–109. DOI: 10.1016/S0099-2399(78)80199-X.
37. Howell RM, Duell RC, et al. The determination of pulp vitality by thermographic means using cholesteric liquid crystals. A preliminary study. Oral Surg Oral Med Oral Pathol 1970;29:763–768. DOI: 10.1016/0030-4220(70)90275-6.
38. Kahan RS, Gulabivala K, et al. Evaluation of a pulse oximeter and customized probe for pulp vitality testing. J Endod 1996;22:105–109. DOI: 10.1016/S0099-2399(96)80283-4.
39. Goho C. Pulse oximetry evaluation of vitality in primary and immature permanent teeth. Pediatr Dent 1999;21:125–127.
40. Gopikrishna V, Tinagupta K, et al. Comparison of electrical, thermal, and pulse oximetry methods for assessing pulp vitality in recently traumatized teeth. J Endod 2007;33:531–535. DOI: 10.1016/j.joen.2007.01.014.
41. Gopikrishna V, Tinagupta K, et al. Evaluation of efficacy of a new custom-made pulse oximeter dental probe in comparison with the electrical and thermal tests for assessing pulp vitality. J Endod 2007;33:411–414. DOI: 10.1016/j.joen.2006.12.003.
________________________
© The Author(s). 2019 Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (https://creativecommons.org/licenses/by-nc/4.0/), which permits unrestricted use, distribution, and non-commercial reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.