ORIGINAL RESEARCH | https://doi.org/10.5005/jp-journals-10024-2680 |
A Cone-beam Computed Tomography Interpretation of Malar Bone Changes in Skeletal Malocclusion
1–5Department of Orthodontics and Dentofacial Orthopedics, Kalinga Institute of Dental Sciences, KIIT Deemed to be University, Bhubaneswar, Odisha, India
6Department of Dental Sciences, District Head Quarter Hospital, Dhenkanal, Odisha, India
Corresponding Author: Bhagabati P Dash, Department of Orthodontics and Dentofacial Orthopedics, Kalinga Institute of Dental Sciences, KIIT Deemed to be University, Bhubaneswar, Odisha, India, Phone: +91 8260521242, e-mail: bhagabatidash23@gmail.com
How to cite this article Dash BP, Reddy R, Mohanty P, et al. A Cone-beam Computed Tomography Interpretation of Malar Bone Changes in Skeletal Malocclusion. J Contemp Dent Pract 2019;20(11):1319–1322.
Source of support: Nil
Conflict of interest: None
ABSTRACT
Aim: The purpose of this cross-sectional study is to signify malar bone anatomy and to obtain linear correlation with varied skeletal pattern by utilizing cone beam computed tomographic views.
Materials and methods: The experimental sample consisted of cone-beam computed tomography (CBCT) scans of 30 patients taken for the purpose of orthodontic treatment and peri implant planning (16 males and 14 females), 11–30 years of age (mean, 23.4 years). The sex and age were documented for all samples and nine landmarks were evaluated. The various CBCT were categorized into different malocclusions based on wits appraisal. Its prevalence was collated with age, sex and various malocclusion by Chi-square test.
Results: Age and gender altogether influenced M1. The mean posterior zygomatic bone width (M1) for all sample was 63.7 mm. For M1 estimations, no huge contrast was observed among left and right side (p = 0.915). The mean anteriorzygomatic bone width (M2) was 51.8 mm. No noteworthy contrast amongst two sides (p = 0.995) or age (p = 0.067) was seen. Although sex altogether influenced M3 variety (p = 0.003), the mean greatest cortical thickness (max CT) (M4) was 9.36 mm, significant difference was observed between the minimum cortical thickness of skeletal class I and skeletal class III malocclusion design.
Conclusion: Detailed evaluation of malar bone should be performed prior to any ortho-surgical procedure using CBCT.
Clinical significance: Our study signifies the importance of consideration of zygoma during any pre-treatment evaluation of skeletal malocclusion. It also marks the pivotal role of zygoma while considering gross facial esthetics. Precise assurance of zygomatic bone size may likewise aid the choice of fitting surgeries and determination of zygomatic implant area.
Keywords: Cone-beam computed tomography, Facial esthetics, Malar bone, Malocclusion.
INTRODUCTION
The zygomatic bone serves as a potential landmark in the assessment of facial aesthetics along with maxilla.1 It is a quadrangular shaped bone surrounded by facial bone, temporal bone and the maxilla. Zygoma anchorage system (ZAS) has lately been the area of interest among orthodontist as it has proven to be potential for securing skeletal anchorage devices that are utilized to assist various tooth movements like distalization of buccal segment in class II cases, intrusion of posterior segment for open bite correction.2 It does not have the disadvantage of anchorage loss. The zygomatic bone (ZB) is also of enormous importance in the field of trauma, reconstruction, and esthetic plastic surgery. There are many studies evaluating the stability of zygomatic skeletal anchorage system in orthodontics.3,4 However, studies limiting to morphological quantitative trait of malar bone are as yet scarce.5,6 Because of the peculiar shape of the malar bone, specific radiological landmarks or planes localization and evaluation on the bone becomes difficult. As the zygoma is used for skeletal anchorage system, its qualitative and quotative evaluation becomes overtly vital in orthodontics and dentofacial orthopedics. Till date cone-beam computed tomography (CBCT) is more routinely performed for the compendious imaging of orthodontic patients than the widely used lateral cephalograms and orthopantomograms. The CBCT scanners came into force about sixteen years ago as an adjunctive technology to meet this need, while decreasing the radiation hazards involved with full CT scans.
CBCT view permits anatomical structures to be properly represented in all three viewing planes. Landmark recognition is also vastly improved in CBCT views with magnification and adaptation in contrast. In 2016, Takamura et al.7 stated that the measurements on lateral skull films obtained from cone beam computed tomographic views were better reproducible than that obtained with lateral cephalogram views.
We hypothesized the anatomy of malar bone is correlated with the skeletal facial pattern; however, we were not able to find studies that estimated this condition in the experimented literature. Basing on our hypothesis and the clinical utility of malar bone and skeletal pattern, the objective of this cross-sectional study is to establish zygomatic bone anatomy and obtain linear co-relation with skeletal facial pattern using cone beam computed tomographic views.
MATERIALS AND METHODS
Study Population and Experimental Design
After Institutional Research and Ethical Committee clearance the study was directed in conformance with the Helsinki declaration of 1975, as revised in 2000. The experimental sample consisted of CBCT scans of 30 patients taken for the purpose of orthodontic treatment and peri implant planning (16 males, 14 females), 11–30 years of age (mean, 23.4 years).
The scans were taken between 2015 and 2017. Scans taken for purpose for evaluation of trauma, pathology or surgical intervention were excluded from the study. Patients with involvement of any syndromes or cleft lip and palate were excluded in the study. 3D CBCT scans were acquired using (My ray, Hyperion X9). The landmark identification and measurement direction used in the study are given in Table 1 and Figures 1A to D. The following standardized measurement (as per Furst et al.8) were recorded 3 times under the supervision of a dentomaxillary radiology specialist.
The skeletal pattern of the skull was estimated using “Wits” estimation of jaw dysplasia. It is a simple strategy wherein the seriousness or level of anterioposterior jaw dysplasia might be estimated on a parallel lateral cephalogram. The technique involves dropping a right angle from point A on the maxilla and point B on the mandible, individually, to the occlusal plane (OP). The point of contact of the perpendiculars to OP is labeled as AO and BO, separately. BO would be situated behind AO in class II skeletal malocclusion, while in class III skeletal malocclusion, BO would be well ahead of AO (Fig. 1E).
| M1 | Posterior zygomatic bone width |
| M2 | Anterior zygomatic bone width |
| M3 | Zygomatic bony projection |
| M4 | Maximum cortical thickness |
| M5 | Minimum cortical thickness |
| M6 | Zygomatic bone height |
| M7 | Pyriform angle |
| M8 | Maxillary angle |
| M9 | Wits appraisal |
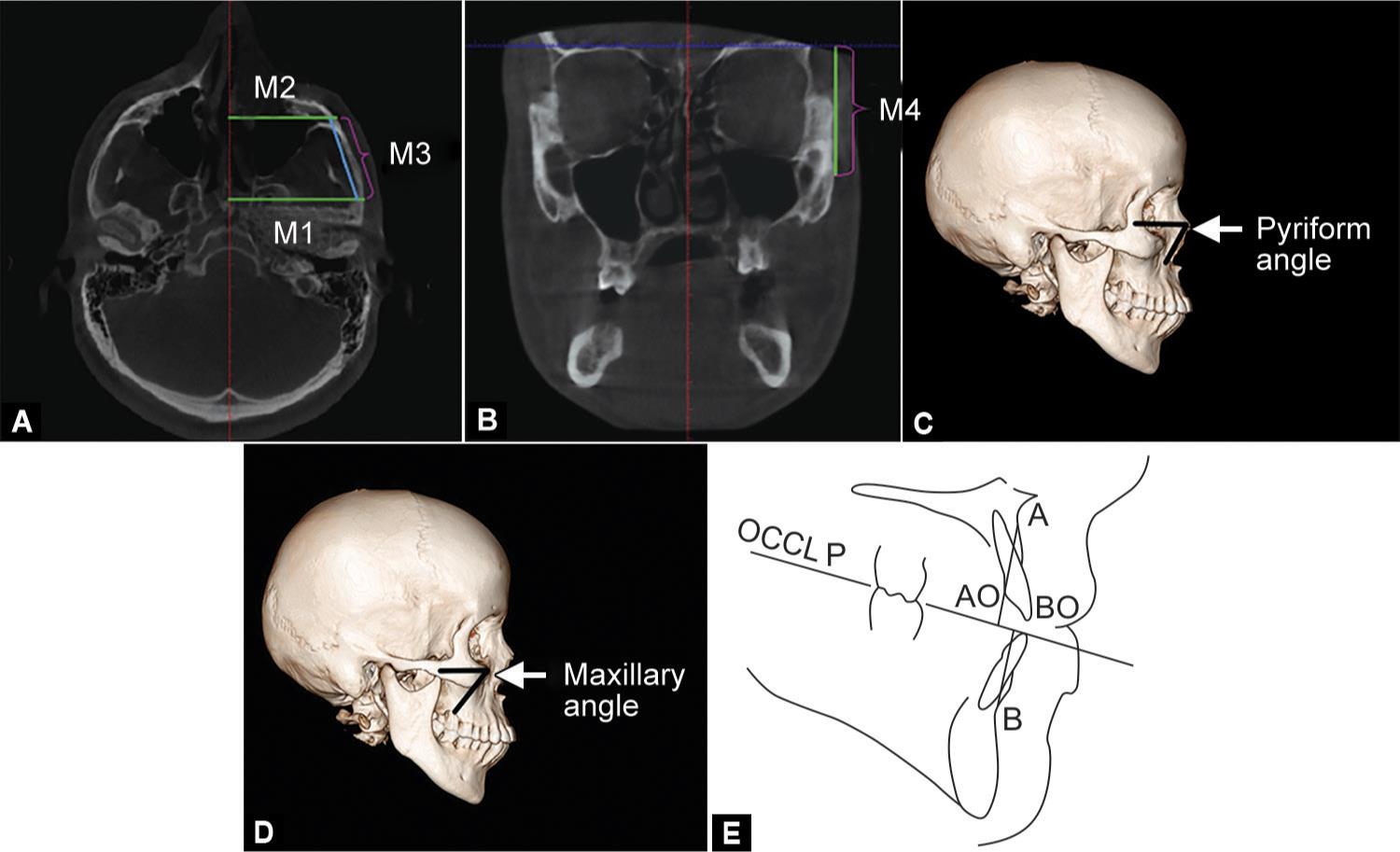
Figs 1A to E: (A) Representative measure of MI, M2, M3; (B) Representative measure of M4; (C) Angular representation of M7; (D) Angular representation of M8; (E) Class III skeletal jaw with point BO ahead of point AO
Statistical Analysis
Statistical analysis was run utilizing statistical package of social sciences (SPSS Version 20; Chicago Inc., USA). The level of significance was fixed at p < 0.05. The Chi-squared test was used to analyze the variation in the mean between three groups of a variable with a normal distribution (Table 2).
RESULTS
In the investigation sample, there were 16 males (42%) and 14 females (58%), in the range of 11 and 30 years (mean age was 23.4 for males and 24.43 for females). The mean of M1 for all patients was 63.7 mm. For M1 estimations, no huge contrast among left and right side (p = 0.915); in any case but, age (p < 0.001) and sexual orientation (p = 0.001) essentially influenced M1 variety. M1 esteems expanded with age. Although significant variation in posterior zygomatic height was observed in different skeletal type.
The M2 was 51.8 mm. For M2 estimations, there was no critical distinction in any factors (right or left side, p = 0.403; age p = 0.846; sexual orientation p = 0.349). The estimation of M3 was observed to be 34.80 mm. No huge distinction in left or right (p = 0.995) or age (p = 0.067) was observed, though sexual orientation altogether influenced M3 variety (p = 0.003). The M4 was 9.36 mm, no critical variation was observed while collating different skeletal malocclusions. No variation was in left or right (p = 0.624) or age (p = 0.534) for M4. Mean M5 values for all the samples were observed to be 4.25 mm, significant distinction was observed between the minimum cortical thickness of skeletal class I and skeletal class III malocclusion design. Mean M6 values were observed 42.60 mm with a standard deviation of 1.92 ± 6.
Significant differences were obtained between class II skeletal patterns and class III skeletal malocclusion patterns. The mean pyriform angle M7 was found to be 59.8°. The pyriform angle was almost comparable in class I and class II skeletal malocclusion with it was significantly reduced in class III malocclusion. Similarly for the maxillary angle (M8) the mean value was found to be 64.0°, significant reduction in degree of maxillary angle was observed between skeletal class II malocclusion pattern and skeletal class III malocclusion pattern (Fig. 2).
| Samples | All | Sk. class I | Sk. class II | Sk. class III | p value | ||||||||||||
|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|---|
| N | Mean | Std. deviation | N | Mean | Std. deviation | N | Mean | Std. deviation | N | Mean | Std. deviation | ||||||
| M1 | 30 | 63.71 | 3.45 | 6 | 63.00 | 2.44 | 16 | 66.11 | 2.15 | 8 | 59.46 | 1.02 | 0.000* | ||||
| M2 | 30 | 51.85 | 2.65 | 6 | 53.03 | 0.82 | 16 | 53.14 | 1.79 | 8 | 48.36 | 1.69 | 0.000* | ||||
| M3 | 30 | 34.80 | 3.17 | 6 | 35.87 | 2.09 | 16 | 35.44 | 3.07 | 8 | 32.74 | 3.39 | 0.091 | ||||
| M4 | 30 | 9.36 | 0.37 | 6 | 9.37 | 0.30 | 16 | 9.41 | 0.43 | 8 | 9.24 | 0.27 | 0.557 | ||||
| M5 | 30 | 4.25 | 0.34 | 6 | 4.45 | 0.35 | 16 | 4.28 | 0.28 | 8 | 4.06 | 0.37 | 0.092 | ||||
| M6 | 30 | 42.60 | 1.92 | 6 | 42.93 | 2.22 | 16 | 43.03 | 1.85 | 8 | 41.49 | 1.55 | 0.159 | ||||
| M7 | 30 | 59.87 | 0.94 | 6 | 60.42 | 0.23 | 16 | 60.39 | 0.25 | 8 | 58.41 | 0.44 | 0.000* | ||||
| M8 | 30 | 64.06 | 0.78 | 6 | 64.03 | 1.00 | 16 | 64.43 | 0.39 | 8 | 63.33 | 0.74 | 0.002** | ||||
| M9 | 30 | 1.87 | 4.44 | 6 | 1.83 | 1.17 | 16 | 5.06 | 1.98 | 8 | −4.50 | 1.60 | 0.000* | ||||
* Signifies a p value less than 0.001
** Signifies a p value less than 0.01
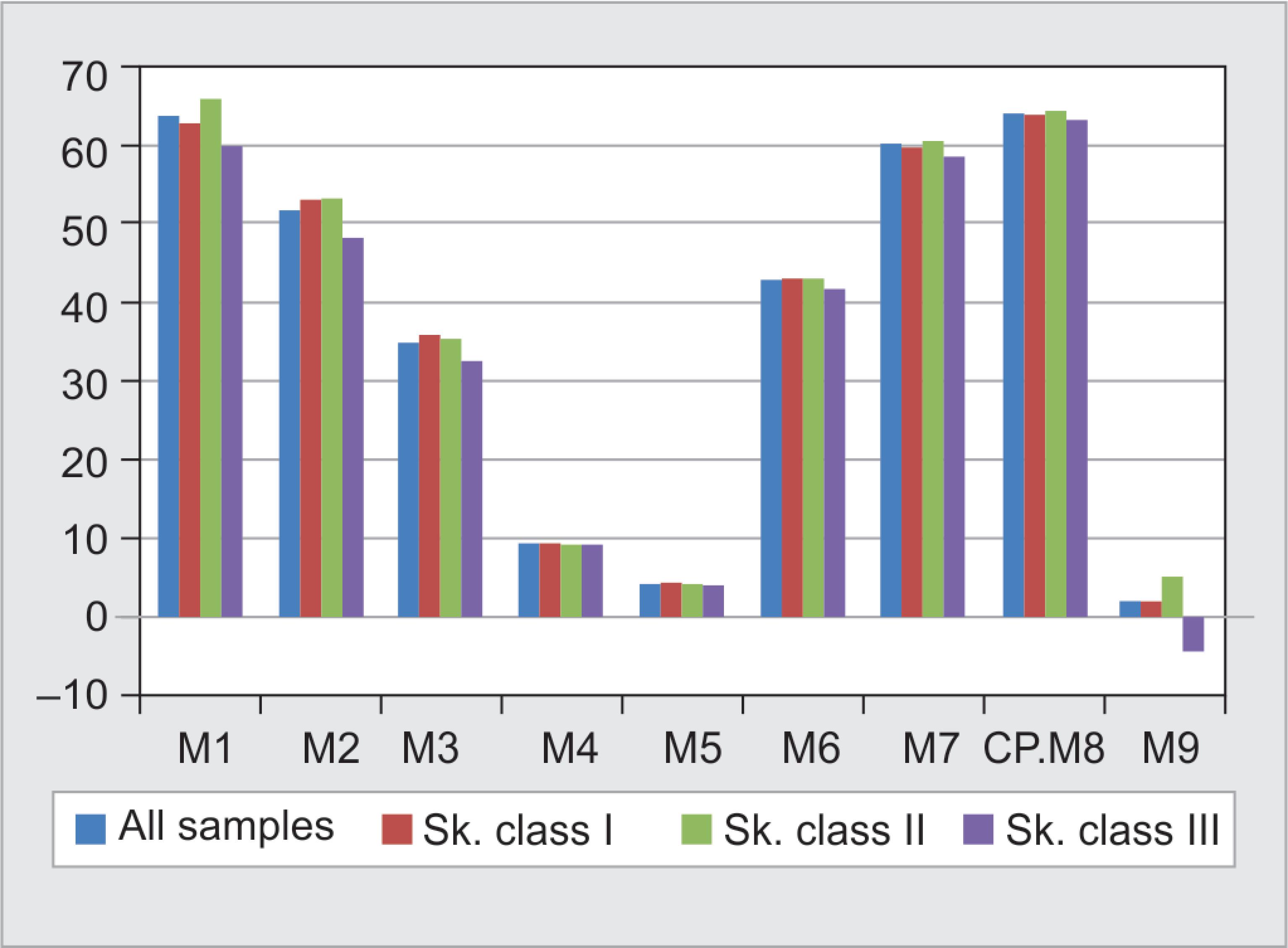
Fig. 2: CBCT values are given according to skeletal malocclusions
DISCUSSION
In the present study we evaluated the radiological parameters of zygomatic bone in correlation with skeletal malocclusion using CT scanned images. Pop culture shows people with increased malar prominence and angular faces are beautiful and fascinating. On the other hand, people with mid face hypoplasia tend to have a hollow mid face leading to greater show of the sclera inferior to the pupil.2,3 We measured the width, depth and pattern of malar bone of various skeletal pattern. Past studies conducted on zygomatic bone mainly evaluated the pneumatization, anatomy and implantation techniques and methods.4,5,9 No study attempted to coordinate the anatomy of zygomatic bone to its facial skeletal pattern. Accurate estimation of malar bone dimensions may aid in choosing suitable surgical interventions and estimating implant position during orthodontic and surgical treatment planning.10
Because of the vicinity between the malar bone and areas with the presence of air as maxillary sinus, ethmoidal sinus, and mastoid air cell framework, many studies were conducted to evaluate the presence of pneumatization of zygomatic bone.11,12 In a study conducted by Nascimento et al.13 ZB was assessed by means of CBCT views to regulate in the event that this bone can deliver attributes like pneumatizations and, in authenticating case to evaluate its dispension with respect to the laterality, age, sex and type. Another form similar to pneumatization in malar bone was observed; however, its commonness was less, i.e., 3.3% of the considered sample and was not clinically significant, therefore evaluation of pattern of pneumatization was not included in our study and we primarily focused on the variation of ZB based on skeletal pattern.
In our study, we opted employing cone beam computed tomography scan because of its accessibility as well as routine use in the center. CBCT computations on subjects at specific length were found to be highly precise and consistent.14 Zygoma has been proven to be a potential site to attain maximum skeletal anchorage. The prospective use of ZB in orthodontics, prosthodontics, oral surgery and plastic surgery is creditable. Here, we utilized the CBCT views in the planes vertical to the zygomatic bone to provide the anatomical data of the zygomatico maxillary complex. Based on the position of the maxillo mandibular jaw base, we divided the cases into three categories (as described in Results). The component of the bone alongside delicate tissues are among the fundamental variables influencing treatment protocol in the malar area.15 For accomplishing facial magnificence there must be balance among the facial promontories. The nose, lips, jaw, glabella, and malar noticeable quality identified with one another and they make a positive perspective inside the face.16,17
In a study conducted by Mendelson et al.18 comparative evaluation of hard and soft tissue midface dimensions of class I and class III individuals using CBCT was performed and he concluded class III males found to have a larger mid face deficiency than class I male. Anterior component of the class III male’s mid face showed posterior positioning. Class I and class III female sample showed similar size and position of the mid facial complex (statistically insignificant). Class III male’s mid facial deficiency was more, mid face complex positioned further laterally and elongated more anteriorly as compared to the class I male and female class III. Zygomatic bone projection was found to be less in class III compared to class I and class II as per our study, thus results of both the studies were in harmony.
The pyriform angle and the maxillary angle have been proven to be pivotal in aging of facial skeleton. Areas with a strong predilection to resorption include mainly the maxilla and the pyriform region of the nose, the superomedial and inferolateral parts of the orbital edge, and the depression in the front of jaws. These regions resorb in a unique and predictable way with maturing. The resultant shortcomings of the skeletal establishment add to the discredit of the maturing face. In patients having congenitally weak skeleton framework, the skeleton might be the primary etiology for the signs of untimely maturing.18 Our study being cross-sectional concluded insignificant changes in the two angles based on differences between facial skeletal pattern. Correlating the soft tissue along with hard tissue of facial skeleton was not included in our study marking as limitation to our project, which can be a subject of further research.
CONCLUSION
Detailed evaluation of malar bone should be performed prior to any ortho-surgical procedure using CBCT. As the treatment protocol varies for different skeletal malocclusions assessing the correlation between hard and soft tissues would become crucial for proper treatment planning.
REFERENCES
1. Capote-Moreno AL, Naval-Gías L, Muñoz-Guerra MF, et al. Zygomatic distraction osteogenesis for correction of midfacial support after hemimaxillectomy: Experience and technical considerations. J Oral Maxillofac Surg 2013;71:e189–e197. DOI: 10.1016/j.joms.2012.11.019.
2. Hinckley RK. Characterisation of malar deficiency in class I and class III individual using CBCT. Saint Louis University; 2012.
3. Schmidseder J. Aesthetic dentistry. University of California Press; 2000.
4. Akan S, Kocadereli I, Aktas A, et al. Effects of maxillary molar intrusion with zygomatic anchorage on the stomatognathic system in anterior open bite patients. Eur J Orthod 2013;35(1):93–102. DOI: 10.1093/ejo/cjr081.
5. Uckan S, Senel F, Arman A, et al. Analysis of zygomatic miniplates for orthodontic skeletal anchorage and evaluation of this system by three-dimensional modelling and finite element analysis. Int J Oral Maxillofac Surg 2007;36(11):1032. DOI: 10.1016/j.ijom.2007.08.247.
6. Kaya, B, Arman, A, Uçkan S, et al. Comparison of the zygoma anchorage system with cervical headgear in buccal segment distalization. Eur J Orthod 2009;31(4):417–424. DOI: 10.1093/ejo/cjp016.
7. Takamaru N, Nagai H, Ohe G, et al. Measurement of the zygomatic bone and pilot hole technique for safer insertion of zygomaticus implants. Int J Oral Maxillofac Surg 2016;45:104–109. DOI: 10.1016/j.ijom.2015.07.015.
8. Furst IM, Austin P, Pharoah M, et al. The use of computed tomography to define zygomatic complex position. J Oral Maxillofac Surg 2001;59:647–654. DOI: 10.1053/joms.2001.23394.
9. Van Vlijmen OJ, Bergé SJ, Swennen GR, et al. Comparison of cephalometric radiographs obtained from cone-beam computed tomography scans and conventional radiographs. J Oral Maxillofac Surg 2009;67(1):92–97. DOI: 10.1016/j.joms.2008.04.025.
10. Uchida Y, Goto M, Katsuki T, et al. Measurement of the maxilla and zygoma as an aid in installing zygomatic implants. J Oral Maxillofac Surg 2001;59:1193–1198. DOI: 10.1053/joms.2001.26725.
11. Carter LC, Haller AD, Calamel AD, et al. Zygomatic air cell defect (ZACD) Prevalence and characteristic in a dental clinic outpatient population. Dentomaxillofac Radiol 1999;28:116–122. DOI: 10.1038/sj.dmfr.4600424.
12. Groell R, Fleischmann B. The pneumatic spaces of the temporal bone: relationship to the temporomandibular joint. Dentomaxillofac Radiol 1999;28:69–72. DOI: 10.1038/sj.dmfr.4600414.
13. Nascimento HAR, Visconti MAPG, Macedo PTS, et al. Evaluation of the zygomatic bone by cone beam computed tomography. Surg Radiol Anat 2015;37:55–60. DOI: 10.1007/s00276-014-1325-3.
14. Kamburoglu K, Kolsuz E, Kurt H, et al. Accuracy of CBCT measurements of a human skull. J Digit Imaging 2011;24:787–793. DOI: 10.1007/s10278-010-9339-9.
15. Mozzo P, Procacci C, Tacconi A, et al. A new volumetric CT machine for dental imaging based on the cone-beam technique: Preliminary results. Eur Radiol 1998;8:1558–1564. DOI: 10.1007/s003300050586.
16. Terino EO. Alloplastic facial contouring by zonal principles of skeletal anatomy. Clin Plast Surg 1992;19(2):487–510.
17. Seimeonow MZ, Sonmez E. Face as an organ: the functional anatomy of the face. The know-how of face transplantation. Ann Plast Surg 2008;61(3):345–352. DOI: 10.1097/SAP.0b013e3181844ea3.
18. Mendelson B, Wong CH. Changes in the facial skeleton with aging: implications and clinical applications in facial rejuvenation. Aesthetic Plast Surg 2012;36(4):753–760. DOI: 10.1007/s00266-012-9904-3.
________________________
© The Author(s). 2019 Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (https://creativecommons.org/licenses/by-nc/4.0/), which permits unrestricted use, distribution, and non-commercial reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.