ORIGINAL RESEARCH | https://doi.org/10.5005/jp-journals-10024-2741 |
Effectiveness of Bubble Breath Play Therapy in the Dental Management of Anxious Children: A Pilot Study
1,3Department of Paedodontics and Preventive Dentistry, Sri Rajiv Gandhi College of Dental Sciences and Hospital, Bengaluru, Karnataka, India
2Department of Paedodontics and Preventive Dentistry, Government Dental College and Research Institute, Victoria Hospital, Bengaluru, Karnataka, India
Corresponding Author: Umme Azher, Department of Paedodontics and Preventive Dentistry, Sri Rajiv Gandhi College of Dental Sciences and Hospital, Bengaluru, Karnataka, India, Phone: +91 9945352984, e-mail: drummeazher@yahoo.com
How to cite this article Azher U, Srinath SK, Nayak M. Effectiveness of Bubble Breath Play Therapy in the Dental Management of Anxious Children: A Pilot Study. J Contemp Dent Pract 2020;21(1):17–21.
Source of support: Nil
Conflict of interest: None
ABSTRACT
Play is an inseparable part of childhood and can act as a mode through which children can be desensitized toward dental treatment.
Aim: To assess and compare the efficacy of bubble breath play therapy (BBPT) and tell-show-do (TSD) technique in the dental management of anxious/fearful children.
Materials and methods: Forty-eight children aged 6–8 years were randomly divided into group I: BBPT and group II: TSD. The effectiveness of the BBPT and TSD technique in reducing anxiety/fear in children was assessed pretreatment, during, and posttreatment evaluation of the child’s anxiety levels using finger pulse oximeter and Venham’s anxiety and behavior rating scale. All children underwent rotary restorative treatment.
Results: The mean pulse rate in the BBPT and TSD group was 106.96 mm Hg and 102.25 mm Hg, respectively, at baseline. A decrease in the pulse rate was observed in both the groups after the application of behavior modification strategies. However, after the dental treatment, the mean pulse rate slightly increased in the BBPT group, while it showed a further improvement in the TSD group.
Conclusion: The BBPT acts as a distraction and can be considered to enhance rapport between the dentist and children during dental treatment.
Clinical significance: Application of appropriate strategies to allay dental fear in children is essential to provide quality dental treatment and build a positive attitude toward oral health.
Keywords: Behavior, Dental anxiety, Dental fear, Play.
INTRODUCTION
Pediatric dentists interact with children of varying age-groups, from infants to adolescents. The primary aim is to provide quality treatment in a safe environment and instill a positive attitude toward dental treatment. However, children often regard dental treatment to be painful; the cause of which can be innate or a previous unpleasant medical or dental experience or vicarious learning. The dental anxiety or fear prevents children from engaging in dental treatment, thereby leading to a negative impact on their dental and general health. According to Armfield, the dental fear/anxiety and avoidance of dental treatment lead to a vicious cycle of dental fear.1 Presence of dental fear/anxiety prevents a child from seeking dental treatment, thereby worsening dental problems, which require more intense and potentially traumatic interventions. This can reinforce or further exacerbate the dental fear/anxiety leading to continued avoidance of dental treatment.
The successful management of these children depends on the ability of the dental practitioner to guide the children through their dental experiences by selecting behavior guidance strategies that will allay their fears and bring about a positive change.
Broadly, nonpharmacologic/psychotherapeutic interventions, pharmacologic interventions, or both can manage dental anxiety. Owing to drawbacks, such as patient safety and cost factor associated with pharmacologic interventions, nonpharmacologic/psychotherapeutic modes of behavior guidance are preferred.
The tell-show-do (TSD) technique based on the principle of learning theory is one of the most commonly used nonpharmacologic methods in pediatric dentistry.2 The technique dictates that before any procedure is done, the child is to be well informed and a demonstration be given using a simulator and the procedure is performed without deviating from the explanation and demonstration. However, as this technique involves only explaining, demonstrating, or observing, it restricts children to only verbal expression and hence a barrier to effective resolution of anxiety issues.
Play is the singular central activity of childhood, occurring at all times and at all places.3 Play therapy can be defined as an interpersonal process where a trained therapist systematically applies the curative powers of play to help the clients resolve their current psychological difficulties and help prevent future ones. The bubble breath play therapy (BBPT) is a simple and concrete relaxation method designed to teach children deep and controlled breathing while creating an awareness in them of their own mind–body connections.4 Hence, as bubble blowing is fun for children, the present study was conducted to assess the effectiveness of BBPT in comparison with the TSD technique in reducing dental anxiety in children following treatment with air motor drill.
MATERIALS AND METHODS
The pilot study was performed after obtaining approval from Institutional Ethical Committee, Sri Rajiv Gandhi College of Dental Sciences, Bengaluru. About 48 children aged between 6 years and 8 years, who visited for their first dental visit with no previous dental experience, were selected. A written informed consent was obtained from patient’s parents after evaluating the medical and dental history of the patient.
Inclusion Criteria
Children with Frankl’s behavior rating 2 and dental caries with a localized enamel breakdown without clinical signs of dentinal involvement (international caries detection and assessment system (ICDAS) score 3) requiring restorations without local anesthesia.
Exclusion Criteria
Children with a previous history of dental treatment, systemic illnesses, physical or intellectual disabilities, and dental caries showing signs of dentinal involvement were excluded.
The children were randomly assigned to two groups (n = 24)—group I (BBPT) and group II (TSD). In group I, the children were given the commercially available bubble breath solutions and asked to blow bubbles. The children were encouraged to blow bigger bubbles. The dental restorations were then rendered using air motor drill. In group II, the children were explained about the procedure in a language they would comprehend and a demonstration was given before the start of the procedure. Following which, without deviating from what was explained and demonstrated, the procedure was performed. In both the groups, child’s anxiety level was assessed by using Venham’s interval rating scale for behavior and anxiety5 and by measuring pulse rate using finger pulse oximeter (Easy care; Model ECPO-250E) at baseline, after the administration of the behavior modification technique, and following dental restorations using an air motor drill.
Statistical Analysis
Mean heart rate was compared between the two groups using unpaired t test. Change of heart rate at different duration was compared between the two groups using unpaired t test after confirming the homogeneity of variance using Levene’s test. Chi-square test was used to compare the behavior and anxiety ratings. Data analysis was performed using software package of statistical analysis (SPSS Inc., Chicago, IL, USA).
RESULTS
A total number of 48 children participated in the study and were allocated between BBPT (n = 24) and TSD (n = 24) groups. Data revealed that both groups were same in demographic characteristics including their sex, mean age, parental education, and age. Levene’s test confirmed the homogeneity of variances.
The mean pulse rate of the patients in both BBPT and TSD groups at baseline, following the administration of behavior modification and dental treatment using airotor is depicted in Table 1 and Figure 1. The mean pulse rate in the BBPT and TSD groups was 106.96 and 102.25 mm Hg, respectively, at baseline. A decrease in the pulse rate was observed in both the groups after the application of behavior modification strategies. However, after the dental treatment, the mean pulse rate slightly increased in the BBPT group (103.5 mm Hg), while it showed a further improvement in the TSD group (93.58 mm Hg) compared to the values following the application of behavior modification strategies.
The comparison of the behavior rating scored using Venham’s interval rating scale for behavior and anxiety of the patients in both the BBPT and TSD groups at baseline, following the administration of behavior modification, and dental treatment using airotor are depicted in Figure 2.
At baseline, all the participants exhibited prominent protest (score 2). After the administration of BBPT and tell-show component of TSD, about 79% in BBPT and 75% of the TSD participants exhibited an improvement in behavior from prominent protest to mild verbal protest. Furthermore, 20.8% of the patients in both groups demonstrated total cooperation. After the dental treatment, about 16.7% of children in the TSD group appeared more relaxed as compared to 4.2% in the BBPT group.
Figure 3 depicts the comparison of the anxiety rating scored using Venham’s interval rating scale for behavior and anxiety of the patients in both BBPT and TSD groups at baseline, following the administration of behavior modification, and dental treatment using airotor. At baseline, the anxiety levels ranged from child appearing scared [(score 2) about 58.3% in both groups] to uneasy and concerned [(score 1) 37.5% in both groups]. About 4.2% of the patients in both groups exhibited reluctance to enter the dental operatory (score 3). Following the application of BBPT and tell-show component of TSD, about 33.3% of the participants in both the groups appeared relaxed, were smiling, and were willing to converse with the dentist (score 1). However, after the dental treatment, the percentage of children who appeared relaxed (25%) was better in the TSD group than that in the BBPT group (4.2%).
DISCUSSION
Children with dental fear and anxiety demonstrate avoidance behavior or delay dental treatment, resulting in deterioration of their oral health. Knowledge on the anxiety levels of children and their oral health is useful for the dentist as it provides an enhanced perspective on the measures to be adopted when treating a pediatric patient and thus be able to implement preconsultation behavior management strategies. Munevveroglu assessed the feelings and attitudes of children toward the dentists and their association with oral health and observed that the mean dmft and the decayed-missing-filled teeth (DMFT) values of children who were afraid of dentists were significantly high.6 A cross-sectional study by Martínez et al. found high levels of fear and anxiety among children for dental treatment.7
In the present study, children’s response to the use of airmotor was assessed, as it is one of the most fear-evoking stimuli. Wardle8 and Lahmann et al.9 observed that dental injection was found to be most powerful as an anxiety-provoking stimulus, followed by the dental drill. Similarly according to Vishwakarma et al., sight, sound, and sensation of the airotor are to be rated as the most fear-eliciting stimuli.10
Response to feared stimulus is multifaceted and has cognitive, physiological, and behavioral dimensions.11 The physiological impact involves activation of the autonomic nervous system (i.e., increased heart rate, blood pressure, and skin conductance) and the limbic–hypothalamic–pituitary–adrenal axis (i.e., release of the stress hormone, cortisol).12
Furlan et al.13 and Carillo-Diaz14 stated that monitoring of heart rate has shown to offer a valid measure of dental anxiety in children. Furthermore, it is sensitive to changes in the level of dental anxiety during the course of treatment. Hence, as pulse rate is a direct measure of physiological arousal and its increase is attributed to stress during dental procedures, it was used to measure the anxiety levels of children in the present study.
| Pulse rate | BBPT | TSD | Mean difference | t | Significant (two tailed) |
|---|---|---|---|---|---|
| Baseline | 106.95 ± 11.16 | 102.25 ± 7.95 | 4.70 | 1.682 | 0.099 |
| After intervention | 102.66 ± 17.41 | 96.08 ± 10.66 | 6.58 | 1.579 | 0.121 |
| After treatment (with airotor) | 103.50 ± 13.52 | 93.58 ± 8.18 | 9.91 | 3.073 | 0.004* |
* Statistically significant

Fig. 1: Mean pulse rate between the groups at different time intervals
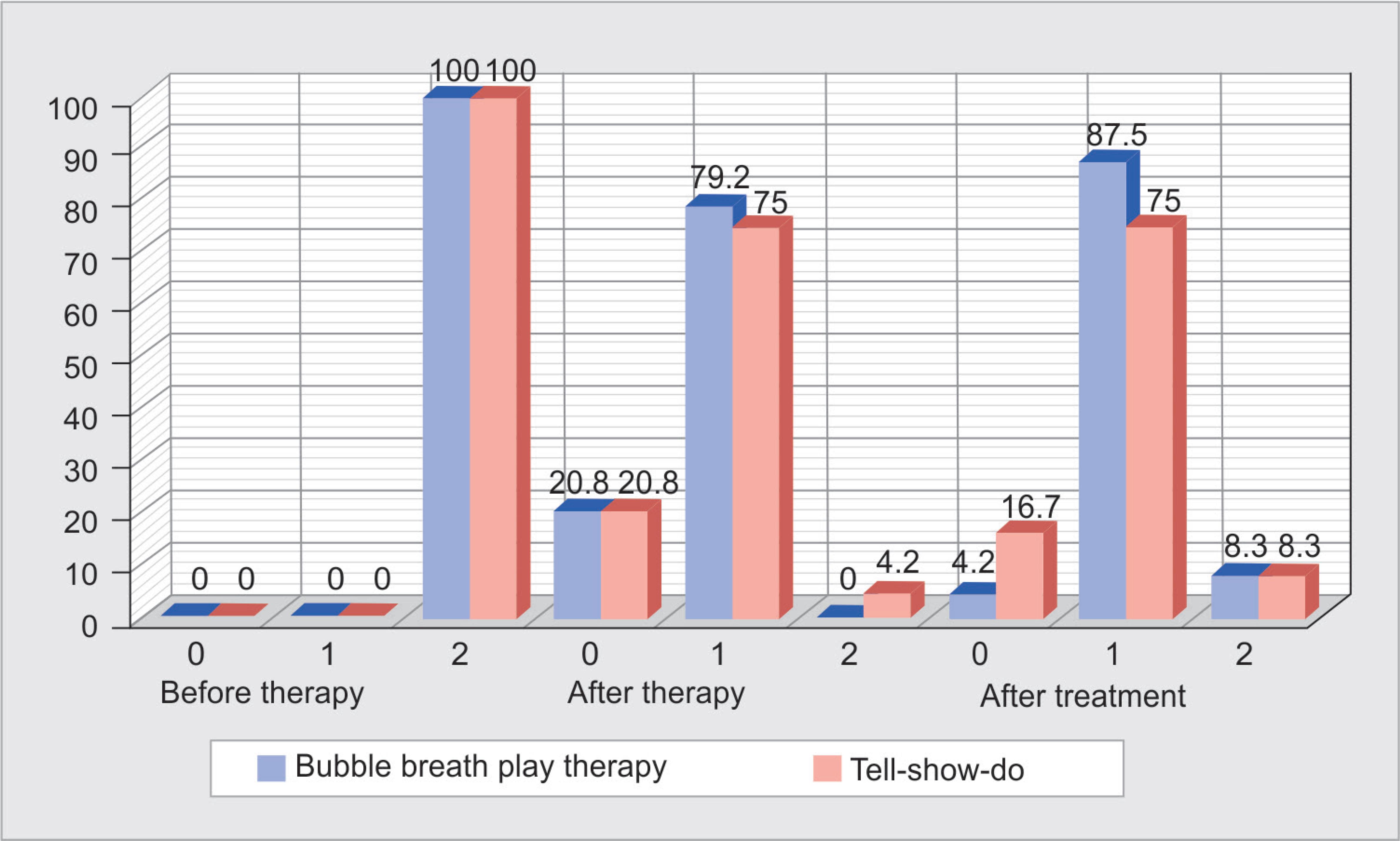
Fig. 2: Comparison of the behavior rating score using Venham’s interval rating scale for behavior and anxiety of the patients in both bubble breath play therapy and tell-show-do group
The TSD technique is the cornerstone of behavior management in pediatric dentistry. The BBPT is a simple, inexpensive, exceptionally engaging and nonthreatening technique. In this technique, the children are encouraged to blow big bubbles and exhale slowly. In an attempt to blow them, they take deep breaths from the stomach. This modality helps to train them in controlled breathing, which physiologically enhances children’s relaxation.
Kiran et al. evaluated the efficacy of BBPT among children (5–10 years) undergoing dental treatment by the graphological method. The BBPT was found to be highly significant in reducing anxiety and distress among children undergoing routine dental procedure.15 In the present study, results showed a reduction in the pulse rate and improvement in the behavior and anxiety ratings following application of BBPT and TSD, compared to the baseline. The pulse rate again slightly increased in the BBPT group compared to the TSD group following the dental treatment with airmotor, indicating an increase in the anxiety levels. However, it was less than the baseline values, indicating a relaxing influence on the anxious child.

Fig. 3: Comparison of the anxiety rating score using Venham’s interval rating scale for behavior and anxiety of the patients in both bubble breath play therapy and tell-show-do group
However, the study’s limitations include a small sample size and inability to generalize the results to a larger population.
CONCLUSION
Within the limitations, it can be concluded that the BBPT acts as a distraction and can be considered a child-friendly method to enhance rapport with the children; however, it does not allay the fears; while the TSD technique is successful in achieving this. Hence, the BBPT can aid in relaxing the child and thereby help in desensitizing the child’s fear by using appropriate behavior shaping strategies.
Further studies on a combination of BBPT and TSD are warranted.
CLINICAL SIGNIFICANCE
- Desensitization of children toward dental treatment is very important in instilling a positive attitude and allaying dental fear.
- Play can be used as a strategy to manage fearful children in a dental clinic and thereby help the dentist to render quality treatment in a safe environment.
- Bubble breath play therapy can help in relaxing the child during dental procedures.
AUTHOR CONTRIBUTIONS
The idea was conceived by Dr Umme Azher and Dr SK Srinath. Data collection by Umme Azher. Data analysis by Dr Umme Azher, Dr SK Srinath and Dr Mihir Nayak. Preparation of manuscript by Umme Azher. Manuscript editing and review by Dr SK Srinath and Dr Mihir Nayak.
REFERENCES
1. Armfield JM, Stewart JF, Spencer AJ. The vicious cycle of dental fear: exploring the interplay between oral health, service utilization and dental fear. BMC Oral Health 2007;7:1. DOI: 10.1186/1472-6831-7-1.
2. Wright GZ, Stigers JI. Non-pharmacologic management of children’s behaviors. In: ed. JA, Dean DR, Avery RE, McDonald ed. Dentistry for the Child and Adolescence.St. Louis: CV Mosby Co.; 2011. p. 30.
3. Landreth G. Play therapy: the art of the relationship,London, England: Routeledge; 2012.
4. Kaduson HG, Schaefer C, ed. 101 more favorite play therapy techniques. Northvale, NJ: Jason Aronson; 2001.
5. Venham LL. Interval rating scales for children’s dental anxiety and uncooperative behavior. Pediatr Dent 1980;2(3):195–202.
6. Munevveroglu AP, Akgol BB, Erol T. Assessment of the feelings and attitudes of children towards their dentist and their association with oral health. ISRN Dent 2014;2014: 867234. DOI: 10.1155/2014/867234.
7. Martínez KR, Zola LMA, Anaya MVM, et al. Fear and anxiety in children treated at the dental surgery of the University of Cartagena. Revista Odontologica Mexicana 2018;22(1):8–14.
8. Wardle J. Fear of dentistry. Br J Med Psychol 1982;55 (Pt 2):119–126. DOI: 10.1111/j.2044-8341.1982.tb01490.x.
9. Lahmann C, Schoen R, Henningsen P, et al. Brief relaxation versus music distraction in the treatment of dental anxiety: a randomized controlled clinical trial. J Am Dent Assoc 2008;139(3):317–324. DOI: 10.14219/jada.archive.2008.0161.
10. Vishwakarma AP, Bondarde PA, Patil SB, et al. Effectiveness of two different behavioral modification techniques among 5-7 year-old children: a randomized controlled trial. J Indian Soc Pedod Prev Dent 2017;35(2):143–149. DOI: 10.4103/JISPPD.JISPPD_257_16.
11. Lang PJ. Fear reduction and fear behavior: problems in treating a construct. In: ed. JM, Shlien ed. Research in psychotherapy, vol. 3 Washington: American Psychological Association; 1968.
12. Nesse RM, Curtis GC, Thyer BA, et al. Endocrine and cardiovascular responses during phobic anxiety. Psychosom Med 1985;47(4):320–332. DOI: 10.1097/00006842-198507000-00002.
13. Furlan NF, Gaviao MB, Barbosa TS, et al. Salivary cortisol, alpha-amylase and heart rate variation in response to dental treatment in children. J Clin Pediatr Dent 2012;37(1):83–87. DOI: 10.17796/jcpd.37.1.n32m21n08417v363.
14. Carrillo-Diaz M, Crego A, Armfield JM, et al. Dental fear related cognitive vulnerability perceptions, dental prevention beliefs, dental visiting, and caries: a cross-sectional study in Madrid (Spain). Community Dent Oral Epidemiol 2015;43(4):375–384. DOI: 10.1111/cdoe.12166.
15. Kiran SDP, Vithalani A, Sharma DJ, et al. Evaluation of the efficacy of play therapy among children undergoing dental procedure through drawings assessed by graphological method: a clinical study. Int J Clin Pediatr Dent 2018;11(5):412–416. DOI: 10.5005/jp-journals-10005-1549.
________________________
© The Author(s). 2020 Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (https://creativecommons.org/licenses/by-nc/4.0/), which permits unrestricted use, distribution, and non-commercial reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.