|
CASE-REPORT |
https://doi.org/10.5005/jp-journals-10024-3301
|
Treatment of Multiple Gingival Recessions Using Modified Tunnel Technique with V-reverse Sutures: A Report of Three Cases
1Department of Periodontology, Government Dental College and Hospital, Mumbai, Maharashtra, India
2,3Faculty of Dental Medicine and Oral Health Sciences, McGill University, Montreal, Quebec, Canada
4Division of Periodontology, Department of Oral Medicine, Infection and Immunity, Harvard School of Dental Medicine, Boston, Massachusetts, United States of America
Corresponding Author: Radhika Chhibber, Faculty of Dental Medicine and Oral Health Sciences, McGill University, Montreal, Quebec, Canada, Phone: +5144431573, e-mail: radhika.chhibber@mail.mcgill.ca
How to cite this article: Tambe LV, Tandale MM, Chhibber R, et al. Treatment of Multiple Gingival Recessions Using Modified Tunnel Technique with V-reverse Sutures: A Report of Three Cases. J Contemp Dent Pract 2022;23(2):232–236.
Source of support: Nil
Conflict of interest: None
Abstract
Aim: The clinical case series presents a minimally invasive modified tunnel procedure with autogenous connective tissue graft (CTG) using a V-reverse sutures to treat multiple gingival recessions.
Background: In periodontal and peri-implant plastic procedures, proper graft and flap stabilization are crucial in the outcomes. The coronally advanced flap allows for better access with the possibility of suturing the graft to the de-epithelialized papillae of the periosteum; there is little evidence with using the V-reverse sutures technique in stabilizing the graft and the flap when performing tunnel techniques (TUN). The following case series presents a minimally invasive modified tunnel procedure with autogenous CTG using V-reverse sutures to treat gingival recessions.
Case description: Three patients with Miller Class I maxillary buccal gingival recessions defects were selected for this study. All subjects were treated with the minimally invasive modified tunnel technique with autogenous subepithelial CTG. V-reverse sutures technique was performed to further improve the stability of the graft at the recipient site. Clinical parameters, including mean recession depth and root coverage esthetic score (RES), were recorded at baseline, 1 week, 2 weeks, 1 month, 3 months, 6 months, and 1-year postoperative follow-up visits.
Conclusion: At the 1-year follow-up, complete root coverage was achieved in multiple gingival recessions defect sites. In conclusion, this technique represents an alternative treatment for Miller Class I gingival recessions defects with clinical and esthetically satisfactory outcomes.
Clinical significance: Combining the advantages of V-reverse sutures and CTG in the treatment of gingival recessions is feasible and noninvasive.
Keywords: Autogenous connective tissue graft, Gingival recessions, Modified tunnel technique.
INTRODUCTION
Gingival recessions defects result in significant esthetic concerns. The prevalence of these defects ranges from 40 to 100% among demographics and populations.1 Therefore, periodontal surgical procedures aim to improve gingival plaque-induced gingival recessions or mucogingival defects.2 However, selecting appropriate surgical techniques plays a critical role in successful clinical outcomes.3,4 Among the plethora of treatment strategies for root coverage, autogenous subepithelial CTG with coronally advanced positioned flap (CAF) was proven to be an effective treatment for multiple gingival recessions defects in areas with esthetic concerns.5 When it comes to perfect blending of color and texture of treated area with surrounding soft tissue, clinicians have frequently used the tunnel technique. The procedure involves creating a partial-thickness flap by undermining the gingival tissue and alveolar mucosa without separating the interdental papillae. Subsequently, the CTG is glided through the tunnel, stabilized to the recipient site, and the flap is coronally positioned. The tunnel technique allows clinicians to reduce the need for vertical incisions, which may enhance the esthetic outcome of the root coverage procedure.6 However, this approach is technique sensitive and challenging to master.7
Other factors suggested in the literature that might influence complete root coverage are positioning the tooth in the arch, the thickness of the gingival biotype, the presence or absence of keratinized tissue, and situations where a tooth is located out of alveolar housing.8 Zucchelli et al. showed the effect of tooth position on complete root coverage.9 Arcoa et al. showed that maxillary teeth are more likely to achieve complete root coverage than mandibular teeth.10 Different surgical techniques, including laterally positioned flap, Zucchelli technique, coronally advanced flap, and double papillae technique, have been described to treat gingival recessions.11 Furthermore, connective tissue graft, donor tissue such as Alloderm (acellular human tissue matrix derived from cadaveric tissue) and Emdogain (gel containing enamel matrix derivates) has also been suggested.12 Among the plethora of techniques, the tunneling technique has the advantage of blood supply from the overlying flap and underlying periosteal bed without compromise in vascularity due to dissection of papillae.13
Along with these minimally invasive techniques, proper stabilization of the graft and flap plays a vital role in surgical outcomes. Previous studies have demonstrated using sling suture techniques with composite resins to promote the close adaptation of the graft and prevent the collapse of soft tissue.1,14,15 There is little evidence available on the stabilization of the CTG when performing modified tunnel procedures. The current case series describe the use of modified tunnel technique with autogenous subepithelial CTG and V-reverse sutures technique to treat multiple gingival recessions defects.
CASES DESCRIPTION
Clinical Case Presentation
All the patients in the case series presented to the Periodontics and Community Dentistry Department of the Government Dental College, Mumbai, India, with esthetic concern and root sensitivity complaints in October 2018. Non-smoker patients with no systemic health diseases, aged between 30 and 40 years, and ability to maintain good oral hygiene were included in this study. Patients had no history of taking antibiotics within 3 months or more than 2 weeks of duration and no gingival surgery within 12 months at the defect site. The clinical examination of the patients revealed Millers Class I gingival recessions defect with #21-22-23 teeth (Fig. 1).

Fig. 1: Millers Class I multiple adjacent recession defects associated with teeth #21-22-23
This case report presents three different clinical cases, respectively: 31-year-old female; 35-year-old male, 38-year-old-male, involving the description of surgical treatment of gingival recessions defects with 1-year follow-ups. Patient selection, consent recordings, and surgical procedure were completed by a single clinician/periodontist at Government Dental College, Mumbai, India.
Recipient Bed Preparation
Composite stops were placed between the contact points of the teeth.2 Local anesthesia (2% Lidocaine with 1:100000 epi) was administered on both recipient and donor sites. Sulcular incision with 15 no. blade was made through each recession area #21-22-23 until the incisal tip of interdental papilla. A full-thickness mucoperiosteal flap was reflected, extending beyond the mucogingival junction to avoid tension in a flap. The tunnel was prepared carefully by gently detaching each pedicle adjacent to the gingival recessions. The undermining of tissues was extended laterally, about 3–5 mm, to prepare the tunnel.
Donor Site Preparation
Subepithelial connective tissue graft from the palate was harvested using the trap door technique. The donor site extended from the distal of the first premolar #24 to the distal of second molar #27. The dimension of the connective tissue graft was 15 mm × 6 mm (Fig. 2). The hemostasis was achieved using saline water-soaked gauze with pressure, followed by a 5–0 vicryl suture.
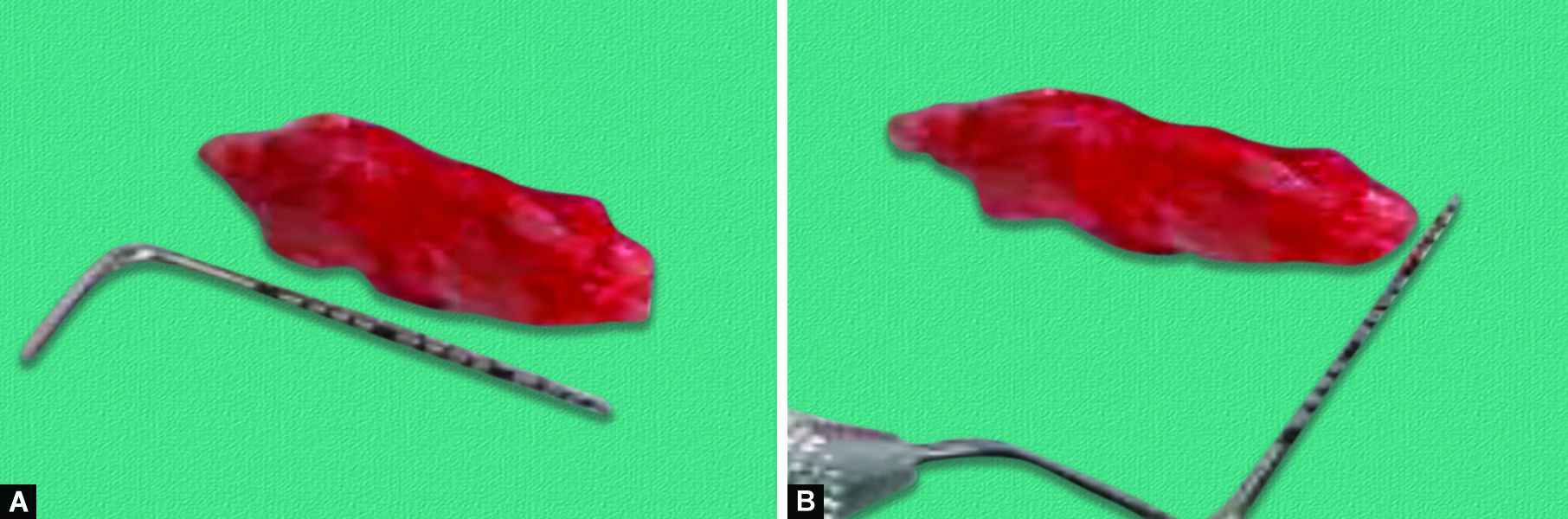
Figs 2A and B: Dimensions of the connective tissue graft (CTG) collected from palate (A) 15 mm in length and (B) 6 mm in width
Suture Placement
The CTG harvested from the palate was carefully glided under the tunnel created between adjacent recession defects.16 With the V-reverse suturing technique, the graft was positioned coronal to CEJ and sutured between the flap and buccal bone (Fig. 3). The V-reverse sutures was started from the palatal side and passed beneath the contact point to the buccal aspect. The needle pierced through the graft and the flap ≈3 mm apical to the free marginal gingiva in the mid-facial region. Then, the needle was passed below the contact point from the palatal side, turned around the splinted composite, and placed a tight knot over the composite (Fig. 3).

Fig. 3: Placement of V-reverse sutures using the splinted contact point between the #21-22-23
Similarly, another suture was placed from other teeth contact point in the mid-facial region ≈2–3 mm away from the last suture. Therefore, each tooth with a recession defect bore one V-reverse sutures and two knots between two contact points. The coronal placement was done with a V-reverse sutures across each flap supported by the interdental composite blobs. The entire surgical area was packed with noneugenol periodontal dressing (Coe-Pak) (Fig. 4).

Fig. 4: Noneugenol periodontal dressing applied (Coe-Pak) on teeth #21-22-23
Postoperative Instructions
An analgesic was prescribed to patients for post-surgical pain relief. They were also instructed to rinse mouth with 0.2% chlorhexidine gluconate twice a day for 2 weeks. The suture placed in the donor site were removed after 1 week. The suture placed on the recipient were removed after 15 days. For supportive periodontal therapy that includes scaling and explanation of oral hygiene maintenance at home, the patients were followed up at regular intervals of 1-week, 1-month, 2-month, 3-month, 6-month, and 12-months postsurgical appointments.
Clinical Outcomes
The periodontal parameters at baseline and the 12-month visit (Fig. 5) together are summarized in Tables 1 and 2. The patient was seen once a week during the first month. After follow-up at 6 and 12 months, a separate clinician evaluated patient satisfaction on the basis of clinical findings (Table 1).

Fig. 5: Twelve month follow-up showing complete root coverage of teeth #21-22-23
| Esthetic score | Before surgery | 1 week after surgery | 2 weeks after surgery | 1 month after surgery | 3 months after surgery | 6 months after surgery | 1 year after surgery |
|---|---|---|---|---|---|---|---|
| (Patient 1) | |||||||
| Gingival margin coverage | 0 | 3 | 6 | 6 | 6 | 6 | 6 |
| Gingival margin contour | 0 | 0 | 0 | 1 | 1 | 1 | 1 |
| Surface texture | 1 | 0 | 1 | 1 | 1 | 1 | 1 |
| Color | 1 | 0 | 0 | 1 | 1 | 1 | 1 |
| (Patient 2) | |||||||
| Gingival margin coverage | 0 | 3 | 3 | 6 | 6 | 6 | 6 |
| Gingival margin contour | 0 | 0 | 0 | 0 | 1 | 1 | 1 |
| Surface texture | 1 | 0 | 0 | 1 | 1 | 1 | 1 |
| Color | 1 | 0 | 0 | 1 | 1 | 1 | 1 |
| (Patient 3) | |||||||
| Gingival margin coverage | 0 | 3 | 3 | 6 | 6 | 6 | 6 |
| Gingival margin contour | 0 | 0 | 0 | 0 | 1 | 1 | 1 |
| Surface texture | 1 | 0 | 0 | 1 | 1 | 1 | 1 |
| Color | 1 | 0 | 0 | 1 | 1 | 1 | 1 |
| Tooth | Initial recession* (mm) | Final recession** (mm) | Total recession reduction (mm) | Total recession reduction (%) |
|---|---|---|---|---|
| 21 | 4 | 0 | 4 | 100 |
| 22 | 4 | 0.5 | 3.5 | 87.5 |
| 23 | 3 | 0 | 3 | 100 |
| Mean ± SD | 3.6 ± 0.53 | 0.1 ± 0.26 | 3.5 ± 0.46 | 95.8 ± 6.66 |
The five variables assessed before the surgery and postsurgical appointments at the 1-week, 1-month, 2-month, 3-month, 6-month, and 12-months post intervals: (1) gingival margin coverage; (2) gingival margin contour; (3) surface texture; (4) color. The mean recession depth was 0.1 ± 0.26 mm recorded after the root coverage procedure. Hence, at a 1-year follow-up, the average root coverage was 3.5 ± 0.46 mm (95.8 ± 6.66 of the preoperative recession). The final comparative analysis was done after 1-year follow-up. As far as esthetic outcome is concerned, the result is satisfactory as per the Root Coverage Esthetic Score (RES) system developed by Cairo et al. given in Table 2.17 The result of this case series shows clinical benefits of V-reverse sutures with modified tunnel technique to treat Miller Class I multiple adjacent gingival recessions defects (Tables 1 and 2).
Follow-up examinations revealed a stable position of the gingiva covering the roots with decreased mucogingival line (GML) (Fig. 5). Recession height (RH) and recession width (RW) were calibrated giving zero. Our results revealed that there was an increase in gingival volume and biotype thickness in teeth #21-22-23 as well as an increase in width of keratinized tissue (WKT) of affected teeth. Each patient was questioned at the last control visit about satisfaction level with regard to the seven main topics including color of gums; contour and shape of gums; dentinal hypersensitivity; root coverage; surgical process (pain during operation and the discomfort related with the total time of the surgery); cost-effectiveness; and postsurgical period (swelling, pain, and postoperative discomforts). The color match and the tissue contour were satisfactory to the patients in all cases as per the Root Coverage Esthetic Score (Table 1). Consequently, this increases the patient satisfaction outcomes.
DISCUSSION
The clinical outcome for treating multiple adjacent gingival recessions defects depends on several factors, including selection of a surgical technique. Given the patient’s spacing between incisors and multiple adjacent recession defects, an envelope tunnel type of flap design would best preserve the midline papilla level with CTG.6 It allows the preservation of intact marginal and papillary tissue while reducing the risk of tissue retraction during healing. Additionally, the modified tunnel technique ensures sufficient blood supply to CTG and maintains its vitality.18 Simultaneously, it maintains the gingival margin harmoniously so that the tunnel technique provides an effective treatment plan, particularly in multiple gingival recessions defects. It also provides an excellent graft adaptation to the recipient site, produces favorable esthetic results, and increases the thickness of keratinized gingiva.19 In contrast, a disadvantage is that the exposed tissue may not have the same color as surrounding tissue.
Another vital factor for the success of periodontal plastic surgery depends on proper suture technique, which allows graft stability and improved flap healing. The sling and interrupted suture are the most commonly performed techniques for CAF. Several other suturing approaches have been described for tunnel technique; for instance, suspensory or double-crossed suture around composite stops allow progression of tunnel flaps coronally.1,20 However, possible drawbacks of such a technique are micromovement of graft and flaps in the midfacial region. Ramírez et al. described V-reverse sutures technique after immediate implant placement to stabilize the CTG and the tunnel flap.16 It has also shown to increase stabilization in midfacial region which may promote better healing.15,16 This case report illustrates modifications of the sling suture technique, i.e., V-reverse sutures, for graft stability while allowing for minimized risk of graft mobility due to muscle movement and allows for the controlled placement and stabilization of the graft coronally over the recipient site.16
Clinicians should select the cases where a minimal 2–3 mm band of keratinized tissue is available. The primary limitation to the success of these cases is the absence of keratinized mucosa and the need for a long-term approach. The V-reverse sutures technique is contraindicated in an area with tension in the recipient flap. The techniques used in our case illustration are relatively simple, quick, and showed excellent patient compliance. Moreover, it improved the stability of the graft and the flap. The V-reverse suturing technique is best suited when the flap is tension-free. V-reverse sutures technique includes but is not limited to: improving stability of the graft and the flap in the midfacial area; reducing flap and graft micromotion; simple, easy, and fast application; and high patient compliance. However, it has to be mentioned that this approach may not be applicable at sites with a thin gingival phenotype or lack of keratinized mucosa since it may cause flap dehiscence.21,22 The V-reverse suturing technique enhances the stabilization of the graft and the flap in the midfacial region which is likely the most crucial area that should be firm for achieving complete root coverage.23 Tunnel technique and V-reverse suturing technique are not recommended in the absence of keratinized mucosa. Clinical studies with long-term outcomes of this approach are needed.
For successful periodontal plastic surgery, patients’ subjective discomfort, gingival thickness (to prevent relapse of GR), and multifaceted esthetic criteria, such as gingival health, harmonious gingival color, and morphological features that include surface texture and gingival contour should be considered. In a further study of the modified tunneling technique and V-reverse suturing technique described herein, these aspects need to be evaluated over the long term.
CONCLUSION
The modified tunnel technique with autogenous CTG improved coronal mobilization of the gingival margin. Furthermore, it was beneficial in meeting esthetic demands and treatment acceptance among the patients. Moreover, the use of V-reverse sutures improved flap and graft stabilization. However, larger clinical trials are required to compare this technique with other conventional methods for the treatment of multiple gingival recessions defects.
Contribution Details
Lashika Tambe designed the concept and drafted the manuscript. Madhura Tandale, Radhika Chhibber and David Wu contributed to the final version of the manuscript.
REFERENCES
1. Vignoletti F, Di Martino M, Clementini M, et al. Prevalence and risk indicators of gingival recessions in an Italian school of dentistry and dental hygiene: a cross-sectional study. Clin Oral Investig 2020;24(2):991–1000. DOI: 10.1007/s00784-019-02996-9.
2. Aroca S, Keglevich T, Nikolidakis D, et al. Treatment of class III multiple gingival recessions: a randomized‐clinical trial. J Clin Periodontol 2010;37(1):88–97. DOI: 10.1111/j.1600-051X.2009.01492.x.
3. Tavelli L, Barootchi S, Cairo F, et al. The effect of time on root coverage outcomes: a network meta-analysis. J Dent Res 2019;98(11):1195–1203. DOI: 10.1177/0022034519867071.
4. Zucchelli G, Tavelli L, McGuire MK, et al. Autogenous soft tissue grafting for periodontal and peri‐implant plastic surgical reconstruction. J Periodontol 2020;91(1):9–16. DOI: 10.1002/JPER.19-0350.
5. Zucchelli G, Tavelli L, Barootchi S, et al. The influence of tooth location on the outcomes of multiple adjacent gingival recessions treated with coronally advanced flap: a multicenter re‐analysis study. J Periodontol 2019;90(11):1244–1251. DOI: 10.1002/JPER.18-0732.
6. Thalmair T, Fickl S, Wachtel H. Coverage of multiple mandibular gingival recessions using tunnel technique with connective tissue graft: a prospective case series. Int J Periodontics Restorative Dent 2016;36(6):859–867. DOI: 10.11607/prd.2278.
7. Zabalegui I, Sicilia A, Cambra J, et al. Treatment of multiple adjacent gingival recessions with the tunnel subepithelial connective tissue graft: a clinical report. Int J Periodontics Restorative Dent 1999;19(2):199. PMID: 10635186.
8. Chambrone LA, Chambrone L. Treatment of Miller Class I and II localized recession defects using laterally positioned flaps: a 24-month study. Am J Dent 2009;22(6):339. PMID: 20178209.
9. Agarwal K, Agarwal K, Gupta K, et al. Zucchelli’s technique combined with platelet-rich fibrin for root coverage. Indian J Oral Sci 2012;3(1):49.
10. Nart J, Valles C, Mareque S, et al. Subepithelial connective tissue graft in combination with a coronally advanced flap for the treatment of Miller Class II and III gingival recessions in mandibular incisors: a case series. Int J Periodontics Restorative Dent 2012;32(6):647. PMID: 23057054.
11. Mutthineni RB, Dudala RB, Ramisetty A. Esthetic root coverage with double papillary subepithelial connective tissue graft: a case report. Case Rep Dent 2014;2014:509319. DOI: 10.1155/2014/509319.
12. Kim DM, Neiva R. Periodontal soft tissue non–root coverage procedures: a systematic review from the AAP regeneration workshop. J Periodontol 2015;86:S56–S72. DOI: 10.1902/jop.2015.130684.
13. Alexiou A, Vouros I, Menexes G, et al. Comparison of enamel matrix derivative (Emdogain) and subepithelial connective tissue graft for root coverage in patients with multiple gingival recession defects: a randomized controlled clinical study. Quintessence Int 2017;48(5):381–389. DOI: 10.3290/j.qi.a38058.
14. Allen EP. Subpapillary continuous sling suturing method for soft tissue grafting with the tunneling technique. Int J Periodontics Restorative Dent 2010;30(5):479. PMID: 20814601.
15. Zadeh HH. Minimally invasive treatment of maxillary anterior gingival recession defects by vestibular incision subperiosteal tunnel access and platelet-derived growth factor BB. Int J Periodontics Restorative Dent 2011;31(6):653. PMID: 22140667.
16. Chacón Ramírez GJ, Tavelli L, Barootchi S, et al. “V‐Reverse” suturing technique for tunnel soft tissue graft and flap stabilization: technique illustration. Clin Adv Periodont 2021;11(3):129–133. DOI: 10.1002/cap.10134.
17. Cairo F, Rotundo R, Miller Jr PD, et al. Root coverage esthetic score: a system to evaluate the esthetic outcome of the treatment of gingival recession through evaluation of clinical cases. J Periodontol 2009;80(4):705–710. DOI: 10.1902/jop.2009.080565.
18. Fahmy RA, Taalab MR. Modified tunnel technique for management of gingival recession in esthetic zone using acellular dermal matrix versus connective tissue graft. Future Dent J 2018. DOI: 10.1016/j.fdj.2018.12.001.
19. Stein JM, Hammächer C. The modified tunnel technique—Options and indication for mucogingival therapy. Journal de Parodontologie et d’Implantologie Orale 2012;31(1):19.
20. Zuhr O, Rebele SF, Vach K, et al. Research Group for Oral Soft Tissue Biology & Wound Healing. Tunnel technique with connective tissue graft versus coronally advanced flap with enamel matrix derivate for root coverage: 2‐year results of an RCT using 3D digital measuring for volumetric comparison of gingival dimensions. J Clin Periodontol 2020;47(9):1144–1158. DOI: 10.1111/jcpe.13328.
21. Rasperini G, Codari M, Limiroli E, et al. Graftless tunnel technique for the treatment of multiple gingival recessions in sites with thick or very thick biotype: a prospective case series. Int J Periodontics Restorative Dent 2019;39(6):e203–e210. DOI: 10.11607/prd.4134.
22. Tavelli L, Barootchi S, Ravidà A, et al. Influence of suturing technique on marginal flap stability following coronally advanced flap: a cadaver study. Clin Oral Investig 2019;23(4):1641–1651. DOI: 10.1007/s00784-018-2597-5.
23. Hiatt WH, Stallard RE, Butler E, et al. Repair following mucoperiosteal flap surgery with full gingival retention. J Periodontol 1968;39(1):11–16. DOI: 10.1902/jop.1968.39.1.11.
________________________
© The Author(s). 2022 Open Access This article is distributed under the terms of the Creative Commons Attribution 4.0 International License (https://creativecommons.org/licenses/by-nc/4.0/), which permits unrestricted use, distribution, and non-commercial reproduction in any medium, provided you give appropriate credit to the original author(s) and the source, provide a link to the Creative Commons license, and indicate if changes were made. The Creative Commons Public Domain Dedication waiver (http://creativecommons.org/publicdomain/zero/1.0/) applies to the data made available in this article, unless otherwise stated.